MOUSE ANTI-COXSACKIEVIRUS B3 ANTIBODY (PV25)
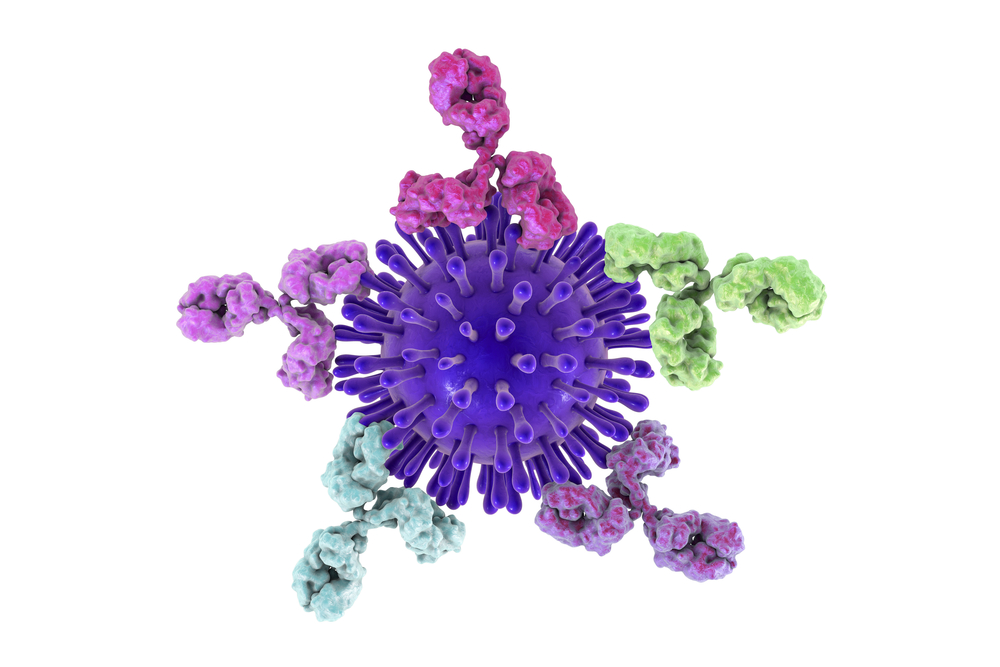
Mouse anti Coxsackievirus B3 Antibody (PV25) is specific for Human Coxsackievirus B3, and shows weak cross-reaction with CVB1 and CVB6. The antibody is suitable for enzyme immunoassay (EIA) applications.
PRODUCT DETAILS – MOUSE ANTI-COXSACKIEVIRUS B3 ANTIBODY (PV25)
- Mouse anti Coxsackievirus B3 (PV25) monoclonal antibody.
- Suitable for immunoassay development.
- Purified by Protein G Sepharose chromatography.
- Presented in phosphate buffered saline, pH 7.4, 0.09% sodium azide.
BACKGROUND
Group B coxsackieviruses (CVBs) are a group of six serotypes of Coxsackievirus and the etiologic agents of a number of human diseases that range in severity from asymptomatic to lethal infections. The various members of the Coxsackie B group were discovered almost entirely in the United States, appearing originally in Connecticut, Ohio, New York, and Kentucky, although a sixth member of the group has been found in the Philippines. However, all six serotypes have a global distribution and are a relatively common cause of gastrointestinal upset.
CVBs are small, single-stranded positive RNA icosahedral viruses that belong to the enterovirus genus of the picornavirus family. The coxsackievirus B3 strain Nancy (CB3) genome is 7396 nucleotides long, and encodes a 2185 amino acid long polyprotein. With only one open reading frame, CVB genome encodes a large polyprotein, which is cleaved into the mature viral proteins by viral proteinases 2A and 3C (Lindberg et al., 1987, Sean and Semler, 2008). CVB capsid is composed of four structural proteins, VP1, VP2, VP3, and VP4. The VP1 protein, which locates on the surface of the capsid, is the main neutralizing antigen of the virus (Muckelbauer and Rossmann, 1997). It exhibits the same gene organization as other enterovirus genomes (Lindberg et al., 1987).
Enterovirus infections have been linked to type 1 diabetes. Type 1 diabetes (T1D) is characterised by the selective loss of insulin producing beta cells from the islets of Langerhans in the pancreas. Affected individuals must administer exogenous insulin throughout their lives. The incidence of the disease is increasing and although previously thought to be a disease of the young, it is now known to develop in all stages of life (Patterson et al., 2009; Thomas et al., 2018). Recent studies confirm that beta cells express specific enteroviral receptors and that they can sustain a productive enteroviral infection. These cells can also mount antiviral responses which attenuate viral replication and may favour the establishment of a persistent enteroviral infection. Together, these responses may combine to create the conditions for enteroviruses to precipitate islet autoimmunity (Richardson and Morgan, 2018).
Enterovirus infection is diagnosed mainly by serological testing e.g. ELISA and from cell culture (Bell et al., 1986; Fields et al., 1985). Because the same level and type of care is given regardless of type of Coxsackie B infection, it is mostly unnecessary for treatment purposes to diagnose which virus is causing the symptoms in question, although it may be epidemiologically useful.
The Native Antigen Company has created a range of enterovirus reagents to help researchers develop better serological testing methods for the diagnosis of enteroviral diseases.
REFERENCES
- Bell et al. (1986). Mu-Antibody capture elisa for the rapid diagnosis of enterovirus infections in patients with aseptic meningitis. Journal of Medical Virology. 19 (3): 213–7.
- Fields, Bernard N.; David M. Knipe; Robert M. Chanock; Joseph L. Melnick; Bernard Roizman; Robert E. Shope (1985). Fields Virology. New York: Raven Press. pp. 739–794.
- Lindberg et al. (1987). Genome of coxsackievirus B3. Virology. Volume 156, Issue 1, Pages 50-63.
- Muckelbauer et al. (1995). The structure of coxsackievirus B3 at 3.5 å resolution. Structure. Volume 3, Issue 7, July 1995, Pages 653-667.
- Sean and Semler (2008). Coxsackievirus B RNA replication: lessons from poliovirus. Curr Top Microbiol Immunol. 323:89-121.
- Patterson et al. (2009). Incidence trends for childhood type 1 diabetes in Europe during 1989–2003 and predicted new cases 2005–20: a multicentre prospective registration study. Lancet, 373, pp. 2027-2033.
- Richardson and Morgan (2018). Enteroviral infections in the pathogenesis of type 1 diabetes: new insights for therapeutic intervention. Current Opinion in Pharmacology. Volume 43, Pages 11-19.
- Thomas et al. (2018). Frequency and phenotype of type 1 diabetes in the first six decades of life: a cross-sectional, genetically stratified survival analysis from UK Biobank. Lancet Diabetes Endocrinol, 6, pp. 122-129.