Infectious diseases are becoming increasingly difficult to manage in the modern medical landscape. Emerging pathogens, mounting antimicrobial resistance, increasing world travel and changing lifestyles have added layers of complexity to controlling and containing infections,1 and so it is critical that laboratories are equipped with the latest technologies and innovations to effectively address current and future outbreaks.
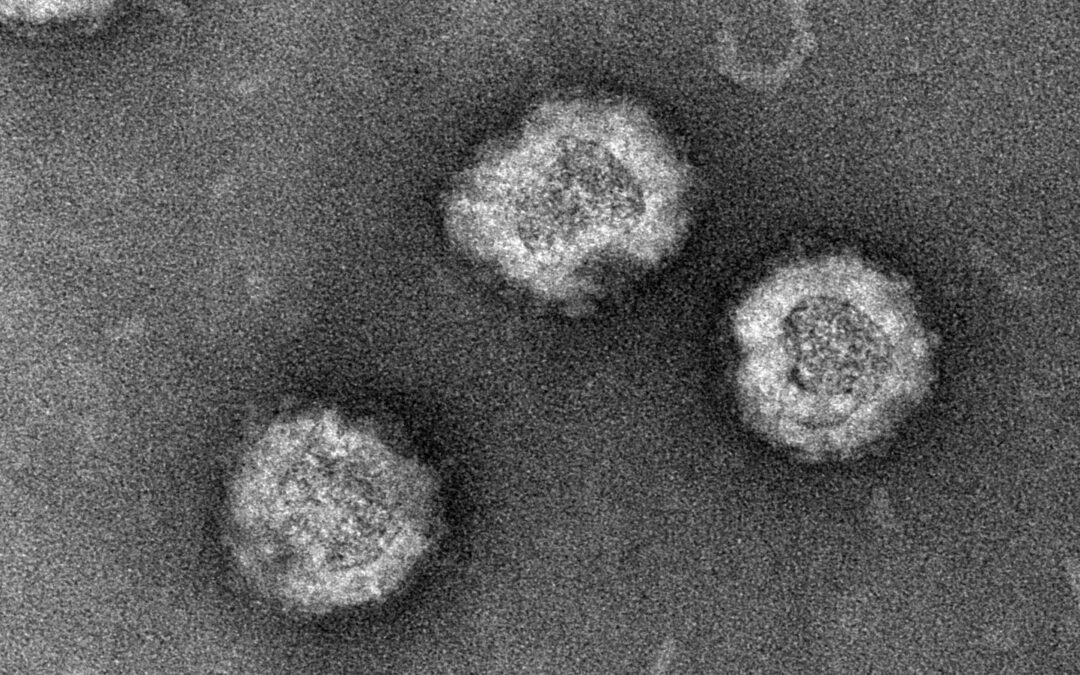
One novel technology that holds great potential for improving infectious disease management is virus-like particles (VLPs). These non-infectious recombinant viral structures perfectly mimic the structure and symmetry of the outer shell of live virions, but lack the genetic material required to productively infect host cells.1,2 Despite being replication-defective and non-infectious, VLPs are recognized, taken up and processed by the immune system in the same way as live viruses, making them ideal candidates for the research and development of diagnostic tests and vaccines.3
Approaches to immunization have advanced significantly in recent years, moving away from the traditional methods based on inactivated or live attenuated viruses.2 The COVID-19 pandemic accelerated this progression, leading to the fast-tracked approval of a new generation of vaccines that includes mRNA-, DNA- and vector-based vaccines, protein subunits and VLPs. These modern vaccines remove whole viruses from the formulation altogether, avoiding the risk of any pathogenic effects.4,5,6
A major benefit of this approach, and VLPs in particular, is that there is no need for the damaging deactivation steps required for cultured native virions, meaning that particles retain their immunogenicity and specificity. VLPs can also be synthesized much faster, taking just 12 to 14 weeks in a variety of expression systems, compared to 24 to 32 weeks for cultivation and deactivation of whole virus particles.2 Furthermore, the production process is both reproducible – preventing batch-to-batch variation that may be found in cultured viral strains – and scalable.7
Rubella is one disease that looks set to benefit from the advantages offered by VLP vaccines in the near future. Immunizing infants and children against the disease via two doses of the measles, mumps and rubella (MMR) vaccine12 has proven to be effective in reducing the incidence of congenital rubella syndrome (CRS) on a global scale.13,10 However, there are several issues when it comes to current management of rubella virus. Firstly, most versions of the rubella vaccine are based on live attenuated virus, and secondly, rubella virus is notoriously difficult to culture and extremely challenging – and therefore costly – to propagate at scale.
Fortunately, rubella VLPs hold huge potential as a scalable, cost-effective route to immunization for vaccine developers, and as a novel platform for rubella research and diagnostics. Recombinant expression of rubella structural polyproteins in mammalian HEK293 cells leads to the self-assembly and secretion of high quality rubella VLPs. This provides researchers with a reliable source of reagents to help them achieve consistent and accurate results throughout vaccine manufacturing. Looking to the future, replacing native rubella products on the market with recombinant VLPs may be the solution that researchers need to meet the World Health Organization’s goal of achieving a world free from measles and rubella infections by 2030.14
VLPs also offer a range of potential applications in diagnostics. Recombinant VLPs stimulate a comparable immune response to native virus particles,3 and have numerous antibody-binding epitopes on their surface, increasing the likelihood of interactions with components of the humoral immune system.8 Consequently, VLP-based enzyme immunoassays have been used to characterize immune responses to a variety of viral diseases in recent years.9
These non-infectious particles have also become important tools in the biomedical field, as they can be engineered to display antigenic epitopes and deliver small molecules to cells and tissues.10 The success of VLPs in research and development has already been demonstrated for a range of viruses – including hepatitis B virus, human papillomavirus (HPV) and hepatitis E virus (HEV)10 – and the technology continues to provide new possibilities for better management of numerous other contagious infections, including rubella.
To learn more download the Virus-Like Particles Factsheet here:
References
1. Excler, JL., et al. 2021. Vaccine development for emerging infectious diseases. Nat Med, 27:591-600. doi: 10.1038/s41591-021-01301-0.
2. Tariq, H., et al. 2022. Virus-like particles: Revolutionary platforms for developing vaccines against emerging infectious diseases. Frontiers in Microbiology, 12. doi: 10.3389/fmicb.2021.790121.
3. Pushko, P., Pumpens, P. and Grens, E. 2013. Development of virus-like particle technology from small highly symmetric to large complex virus-like particle structures. Intervirology, 56(3):141-165. doi: 10.1159/000346773.
4. Gupta, R. et al. 2023. Platforms, advances, and technical challenges in virus-like particles-based vaccines. Frontiers in Immunology, 14. doi: 10.3389/fimmu.2023.1123805.
5. Fuenmayor, J., Gòdia, F. and Cervera, L. 2017. Production of virus-like particles for vaccines. New Biotechnology, 39:174-180. doi: 10.1016/j.nbt.2017.07.010.
6. Dai, S., Wang, H. and Deng, F. 2018. Advances and challenges in enveloped virus-like particle (VLP)-based vaccines. Journal of Immunological Sciences, 2(2):36-41. doi: 10.29245/2578-3009/2018/2.1118.
7. Nooraei, S. et al. 2021. Virus-like particles: preparation, immunogenicity and their roles as nanovaccines and drug nanocarriers. J Nanobiotechnol 19(1):59. doi: 10.1186/s12951-021-00806-7.
8. Mohsen, M. et al. 2018. Interaction of viral capsid-derived virus-like particles (VLPs) with the innate immune system. Vaccines, 6(3):37. doi: 10.3390/vaccines6030037.
9. Lundstig, A. and Dillner, J. 2006. Serological Diagnosis of Human Polyomavirus Infection. In: Advances in Experimental Medicine and Biology. New York: Springer. doi: 10.1007/0-387-32957-9_7.
10. Qian, C. et al. 2020. Recent progress on the versatility of virus-like particles. Vaccines, 8(1):139. doi: 10.3390/vaccines8010139.
11. Das, PK. and Kielian, M. 2021. Molecular and structural insights into the life cycle of rubella virus. Journal of Virology, 95(10). doi: 10.1128/jvi.02349-20.
12. Haldeman-Englert, C., Turley, R. and Novick, T. TORCH panel. Health Encyclopedia. University of Rochester Medical Center. Available at: https://www.urmc.rochester.edu/encyclopedia/content.aspx?ContentTypeID=167&ContentID=torch_panel.
13. Rubella vaccines: WHO position paper – July 2020. 2020. Weekly Epidemiological Record, No 27. World Health Organization. Available at: https://apps.who.int/iris/bitstream/handle/10665/332952/WER9527-306-324-eng-fre.pdf?sequence=1.
14. Kauffmann, F. et al. 2021. Measles, mumps, rubella prevention: How can we do better?. Expert Review of Vaccines, 20(7):811-826. doi: 10.1080/14760584.2021.1927722.