Cryptosporidium
Cryptosporidium Background
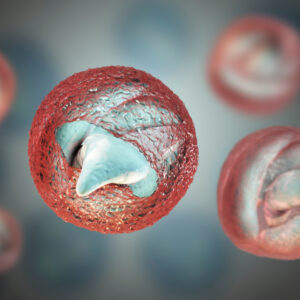
Cryptosporidium is a major waterborne parasites worldwide and causes cryptosporidiosis, an infection that may present as a diarrhoeal with or without a persistent cough in immunocompetent hosts (Bouzid et al., 2013). The first cases of human cryptosporidiosis were reported in 1976 in patients with severe watery diarrhea. In humans, the main causes of disease are C. hominis and C. parvum which account for more than 90% of human cases of cryptosporidiosis. Cryptosporidium is a single-celled eukaryote, a member of the protist phylum Apicomplexa which includes other apicomplexan pathogens such as the malaria parasite Plasmodium and the toxoplasmosis parasite Toxoplasma. Unlike Plasmodium, which transmits via a mosquito vector, Cryptosporidium does not use an insect vector, and is capable of completing its lifecycle within a single host, resulting in cyst stages that are excreted in feces or through inhalation of coughed on fomites and are capable of transmission to a new host. Cryptosporidiosis is typically an acute, short-term infection, can be recurrent through reinfection in immunocompetent hosts, and become severe or life-threatening in immunocompromised individuals. In humans, it remains in the lower intestine and may remain for up to five weeks. Cryptosporidium has three developmental stages: meronts, gamonts and oocysts. They reproduce within the intestinal epithelial cells. The Cryptosporidium spore phase (oocyst) can survive for lengthy periods outside a host and can resist many common disinfectants, notably chlorine-based disinfectants. The parasite is transmitted by these environmentally hardy cysts (4–6 μm in size) that, once ingested, exist in the small intestine and result in an infection of intestinal epithelial tissue. Transmission by ingestion or inhalation of coughed on fomites is a second, less likely route of infection. Currently, there is only one drug available to treat cryptosporidiosis, nitazoxanide, which is largely ineffective for those that most need treatment, namely malnourished children and immunosuppressed patients, such as HIV/AIDS patient (Gibson & Striepen, 2018).
References
- Bouzid M, Hunter PR, Chalmers RM, Tyler KM. Cryptosporidium pathogenicity and virulence. Clin Microbiol Rev. 2013 Jan;26(1):115-34.
- Gibson AR, Striepen B. Cryptosporidium. Curr Biol. 2018 Mar 5;28(5):R193-R194.
Cryptosporidium Antigens
Cryptosporidium Antibodies
Questions?
Check out our FAQ section for answers to the most frequently asked questions about our website and company.