Plasmodium
Malaria is a life-threatening disease that affects millions of people worldwide and is caused by Plasmodium parasites that are transmitted through the bite of an infected female mosquito of the Anopheles species. Five species of Plasmodium are known to cause malaria in humans. Most cases of malaria are caused by P. falciparum and P. vivax, but reports suggest that cases caused by P. knowlesi are on the increase in Malaysia. Early symptoms of malaria are non-specific and therefore accurate laboratory diagnosis and early treatment is essential to prevent disease progression and death.
Plasmodium Background
Malaria is an infectious disease caused by obligate intracellular protozoan parasites of the genus Plasmodium which are transmitted to humans through the bite of infected female mosquitoes of the Anopheles species. Five different species of Plasmodium are known to cause disease in humans including P. falciparum, P. vivax, P. ovale, P. malariae and P. knowlesi. Malaria is a globally widespread disease affecting 100 countries, with most cases occurring in African regions and the Americas. In African regions, P. falciparum causes the majority of malaria cases, whereas P. vivax is the predominant cause of malaria in regions of the Americas (WHO). Cases of malaria caused by P. ovale and P. malariae are uncommon or rare. However, cases of malaria caused by P. knowlesi are common in Malaysia and are reported to be on the increase (Barber, BE).
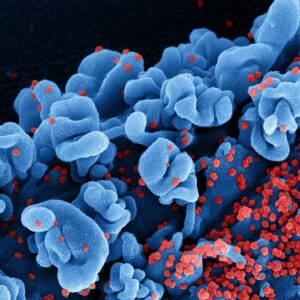
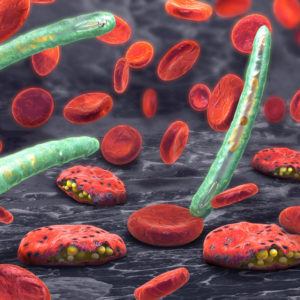
Many different species of Anopheles mosquitoes have been identified as vectors for malaria and the species can vary according to geographical location. The Anopheles mosquitoes, causing most cases of malaria, bite from dawn until dusk and lay their eggs in shallow water, which develop into larvae and then emerge as adults. Humans can develop malaria after a single bite from an infected female mosquito. As the mosquito takes a blood meal, sporozoites are injected into the human bloodstream, which then infect hepatocytes in the liver and multiply. The schizonts that develop in the liver eventually rupture releasing merozoites that invade red cells and enter the erythrocyte cycle of development. The parasites then go through a replication cycle within erythrocytes, leading to the eventual rupture of the cells and release of toxins that cause the febrile illness that is characteristic of Malaria. If left untreated, merozoites can replicate to produce gametocytes which can infect susceptible mosquitoes during a bloodmeal.
Malaria can develop over a period of 7 to 18 days. In uncomplicated cases, the symptoms of malaria include fever, general malaise, nausea, chills, myalgia and headache. In cases of severe malaria clinical symptoms including confusion, acidosis, hypoglycaemia, anaemia, renal impairment and jaundice. If left untreated, cases of severe malaria can worsen leading to coma and death. The progression of the disease to severe malaria can depend on many factors including the species of the Plasmodium involved, the age of the individual, immune status, correct diagnosis and availability of treatment (WHO).
A quick and accurate diagnosis of malaria is essential prior to treatment to prevent progression to severe disease and to reduce the reservoir of parasites in the human population. Diagnosis of malaria is currently based on clinical symptoms, blood film for malaria parasites (BFMP), polymerase chain reaction (PCR) and rapid diagnostic test (RDT). The most effective treatment for malaria caused by P. falciparum is an artemisinin-based combination therapy (ACT), while chloroquine is the preferred option for P. vivax and P. ovale infection in areas without chloroquine-resistance. A vaccine providing partial protection against malaria is currently in development with pilot studies taking place in 2019 (WHO).
References
- World Health Organization: Malaria. Key facts
- Barber BE, Rajahram GS, Grigg MJ, William T, Anstey NM. 2017. World Malaria Report: time to acknowledge Plasmodium knowlesi malaria. Malar J. Mar 31;16(1):135
- World Health Organization: Malaria. Overview of Malaria treatment
Plasmodium Antigens
Our range of Plasmodium antigens includes Plasmodium falciparum Aldolase, Lactate Dehydrogenase and Histidine-Rich Protein II, as well as Plasmodium vivax Lactate Dehydrogenase.
Mouse Anti-Plasmodium Falciparum HRP-2 Antibody (M302)
Price range: $454.04 through $1,139.31 excl. VAT
Mouse Anti-Plasmodium Falciparum HRP-2 Antibody (M303)
Price range: $454.04 through $1,139.31 excl. VAT
Mouse Anti-Plasmodium Falciparum HRP-2 Antibody (M482)
Price range: $454.04 through $1,139.31 excl. VAT
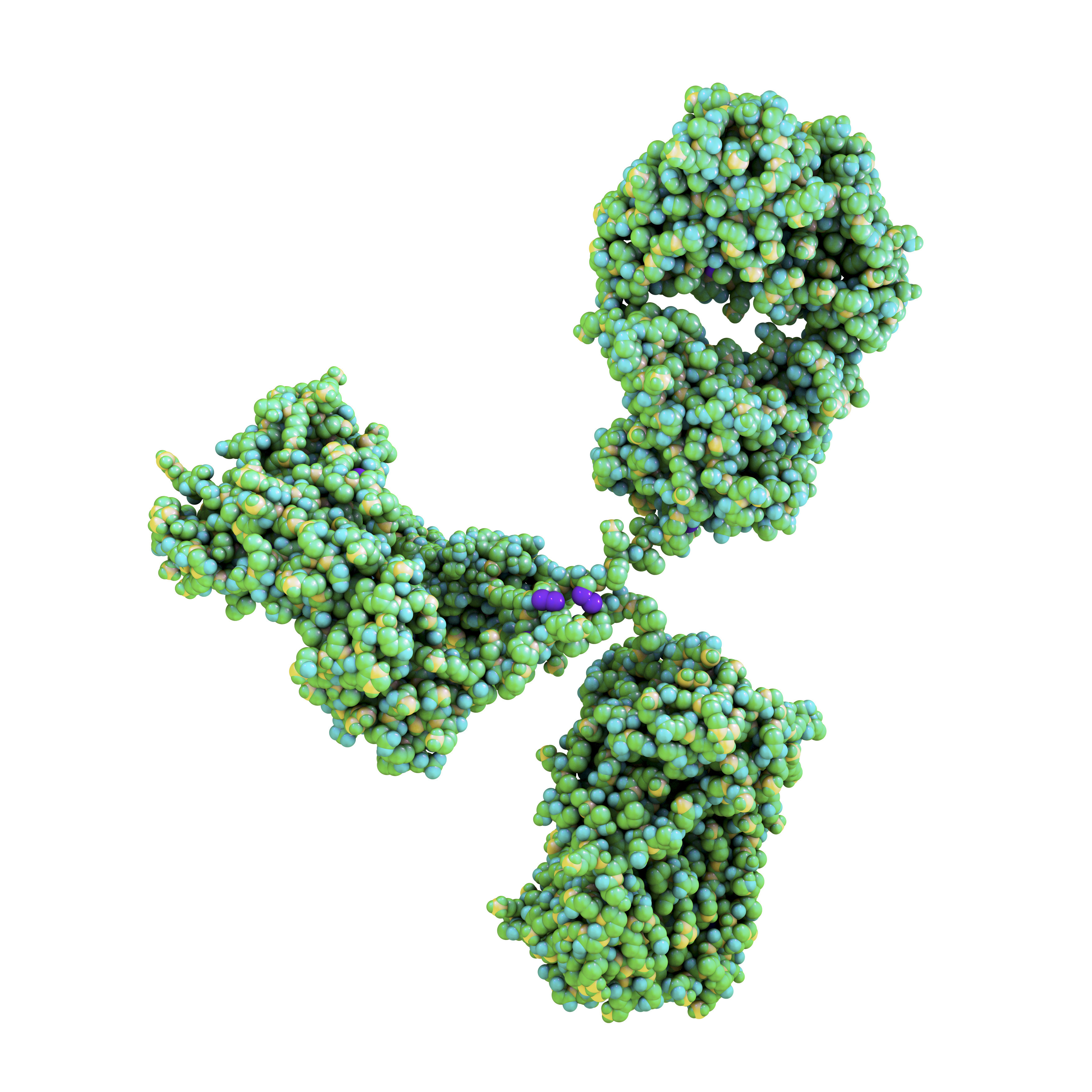
Plasmodium Antibodies
Our range of Plasmodium specific antibodies includes reagents suitable for detecting Plasmodium falciparum HRP2, and Plasmodium vivax Lactate Dehydrogenase. The range includes matched pair antibodies suitable for assay development for ELISA and Lateral Flow applications
Questions?
Check out our FAQ section for answers to the most frequently asked questions about our website and company.