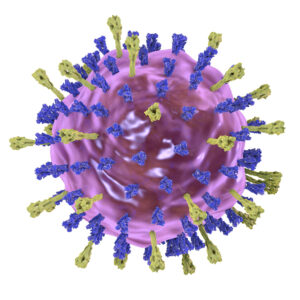
Varicella-Zoster Virus
Varicella-Zoster Virus Background
Varicella occurs worldwide and is endemic in populations of sufficient size to sustain year-round transmission, with epidemics occurring every 2–3 years. It shows a strong seasonal pattern, with peak incidence during winter and spring or during the cool, dry season. VZV infections are species-specific to humans, but it can survive in external environments for a few hours (Gershon et al., 2015). The epidemiology of the disease differs between temperate and tropical climates. The reasons for the differences are poorly understood and may relate to properties of VZV (known to be sensitive to heat), climate, population density and risk of exposure (e.g., attendance at childcare facility or school or the number of siblings in the household) (WHO).
The virus is highly communicable and spreads by the airborne route, with an extremely high transmission rate in temperate countries. Most virus comes from skin where it is highly concentrated in vesicles; indeed, skin cells and cell-free VZV are frequently shed and are probably the major source of infectious cell-free airborne virus. Infected children without skin lesions are not contagious to others (Gabutti et al., 2016).
VZV causes two human diseases, varicella (chickenpox) and herpes zoster (shingles). Chickenpox (varicella), is a disease most commonly affecting children, teens, and young adults, and shingles (herpes zoster) in adults; shingles is rare in children. VZV multiplies in the lungs, and causes a wide variety of symptoms. Varicella is generally self-limited and vesicles gradually develop crusts, which disappear over a period of 7-10 days. Individuals remain contagious until all lesions have crusted over. The disease is typically mild, but severe complications may arise, including bacterial infections (e.g. cellulitis, pneumonia) and neurological complications (e.g. encephalitis), and these can be fatal. Disease is associated with higher morbidity and mortality in infants and in individuals with an impaired immune system (WHO). Herpes zoster is a reactivation of a latent VZV infection. After the primary infection (chickenpox), the virus lies dormant in the nerves, including the cranial nerve ganglia, dorsal root ganglia, and autonomic ganglia. Many years after the person has recovered from chickenpox, VZV can reactivate to cause neurological conditions. Antiviral drugs and vaccines against both varicella and zoster are available and are effective in treating and preventing VZV-induced disease (Gabutti et al., 2016). Multiple vaccine formulations of the live attenuated vaccine, based on the Oka VZV strain, have been available since 1974 and Varicella vaccines are available as a single antigen and in combination with measles, mumps and rubella vaccine.
References
- Gabutti G, Franchi M, Maniscalco L, Stefanati A. Varicella-zoster virus: pathogenesis, incidence patterns and vaccination programs. Minerva Pediatr. 2016 Jun;68(3):213-25.
- Gershon AA, Breuer J, Cohen JI, Cohrs RJ, Gershon MD, Gilden D, Grose C, Hambleton S, Kennedy PG, Oxman MN, Seward JF, Yamanishi K. Varicella zoster virus infection. Nat Rev Dis Primers. 2015 Jul 2;1:15016.
- WHO. Immunization, Vaccines and Biologicals. Varicella.
Varicella-Zoster Virus
Questions?
Check out our FAQ section for answers to the most frequently asked questions about our website and company.