Human Coronavirus
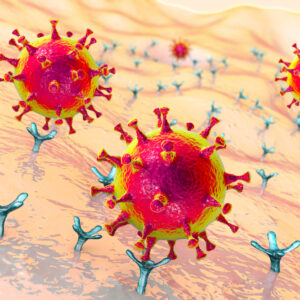
Coronaviruses were first identified in the mid-1960s and are named after the crown-like spikes on their surface. There are six different coronaviruses which can infect humans and cause illness. These comprise the four common coronaviruses; 229E and NL63 (alpha coronaviruses), OC43 and HKU1 (beta coronaviruses), and two other coronaviruses, MERS-CoV and SARS-CoV, both of which can cause severe illness and remain a significant public health concern. A new coronavirus, SARS-CoV-2 was identified in December 2019 in Wuhan City, Hubei Province of China and is the causative agent of the COVID-19 respiratory disease, which was declared a pandemic in March 2020.
The Native Antigen Company offers recombinant antigens and monoclonal antibodies for research into coronaviruses. We are also able to undertake a wide range of custom projects on your behalf. More information on our services can be found here.
Human Coronavirus Background
People around the world commonly get infected with human coronaviruses 229E, NL63, OC43, and HKU1. However, occasionally coronaviruses that infect animals can evolve to become a new human coronavirus. Examples include SARS-CoV and MERS-CoV (CDC), as well as the current outbreak of SARS-CoV-2 (formerly Novel Coronavirus 2019-nCoV).
Severe acute respiratory syndrome (SARS) is a lower respiratory tract illness that was first reported in patients from the Guandong Province of China, in November 2002. The causative agent, which was previously unknown, was isolated in 2003 and named as SARS coronavirus (SARS-CoV). The SARS coronavirus is an enveloped, single-stranded, positive RNA virus of the family, Coronoviridae (NCBI). The virus is thought to have a zoonotic origin, with the horseshoe bat being the primary natural reservoir, but this has not yet been confirmed. Mammals, including the palm civet, may act as intermediate hosts. In 2003, the SARS coronavirus spread rapidly and affected over 8,000 people in 26 countries. The rapid spread of SARS-CoV is thought to be due to person-to-person transmission of the virus via aerosol droplets or close contact with infected individuals. Since 2012, MERS-CoV has caused over 800 deaths in 27 countries with Saudi Arabia being the most affected (reviewed in Xu et al., 2019). The symptoms of SARS infection are like influenza and include fever, malaise, muscle pain, headache, diarrhoea and shivering. Clinical symptoms may also include coughing and shortness of breath. Respiratory distress may rapidly develop in some patients, resulting in death. SARS has a high rate of mortality and resulted in 774 deaths during the first epidemic in 2003. Currently, no licenced vaccine is available for the prevention of SARS infection. SARS continues to be of global health concern due to the rapid spread of the virus, the high mortality rate and the fears of a future SARS outbreak (WHO)
Middle East respiratory syndrome coronavirus (MERS-CoV) was first reported in 2012 after genome sequencing of a virus isolated from human sputum samples taken from a patient with flu-like symptoms and it has since spread rapidly (Al-Amri et al., 2017). Since 2012, MERS-CoV has caused over 800 deaths in 27 countries with Saudi Arabia being the most affected (Hashem et al., 2019). It is an acute respiratory disease and often leads to pneumonia and renal failure, very similar to severe acute respiratory syndrome (SARS) caused by another coronavirus, SARS-CoV. Like SARS-CoV, MERS-CoV is a zoonotic virus transmitted from animals to humans. The evolutionary origins of MERS-CoV are unknown but evidence suggests that insectivorous bats are likely to be the original source (Anthony et al., 2017). MERS-CoV and its neutralizing antibodies have also been detected in dromedary camels, which act as a reservoir host (Reusken et al., 2013) and both bat-to-human and camel-to-human transmission is possible. MERS-CoV is one of several viruses identified by WHO as a likely cause of a future epidemic and is listed for urgent research and development. The high case fatality rate, vaguely defined epidemiology, and absence of prophylactic or therapeutic measures against this novel virus have created an urgent need for an effective vaccine should an outbreak expand to pandemic proportions.
In late December 2019, officials in Wuhan (Hubei province), China announced that 27 residents, mostly stallholders at the city’s Huanan Seafood Market, had fallen ill with an unknown virus. A week later they confirmed that 44 patients were infected with the virus. The virus was isolated from a patient several days later and the genetic sequence was made available to the WHO; in the interim the virus was named Novel Coronavirus (2019-nCoV) and was then subsequently named SARS-CoV-2 (Hui et al., 2020). Later investigations reported that individuals from Hubei province may have shown symptoms as early as November 2019. SARS-CoV-2 is a new strain of coronavirus that has not been previously identified in humans and also not been previously detected before the outbreak was reported in China. The virus shows ~79% identity at the sequence level to SARS coronavirus and genomic sequencing has shown that it is most closely related to betacoronaviruses of bat origin, suggesting that these animals are the likely reservoir hosts for this emerging viral pathogen (Lu et al., 2020). However, it is believed that human infection may have occurred through an intermediate host, such as the Pangolin. The substantial increase in cases thereafter has been due to human-to-human transmission of the virus. By end of February 2020, new cases were reducing in China but subsequently increased dramatically in a number of other countries including Italy, Iran, and South Korea (WHO, 2020). On March 11 2020, SARS-CoV-2 was declared a pandemic (WHO, 2020). Although SARS-CoV-2 displays some similar mechanics of infection and symptoms to SARS, there is still much unknown about this virus, including reservoir species, the transmission route, the incubation period and characteristics of the susceptible population and survival rates (Hui et al., 2020). Illnesses associated with SARS-CoV-2 are similar to several other respiratory diseases and show the typical features of viral pneumonia, including fever, dry cough, sore throat and headache. Most cases are considered mild to moderate with a subset experiencing more severe illness with shortness of breath and difficulty breathing. There is believed to be substantial under reporting of cases, particularly among those with milder symptoms. The elderly are particularly at risk, especially those with pre-existing health conditions including cardiovascular diseases and diabetes, and most deaths have been in those over 60 years of age. The sequence WIV04/2019 is thought likely to be the original sequence infecting humans and several notable variants of this have been identified to be of particular importance. D614G is a SARS-CoV-2 variant with a mutation in the spike protein, which has increased in frequency during the pandemic and is reportedly more infectious, becoming the dominant form in the pandemic. Other variants have also raised concern including those containing a change from asparagine (N) to tyrosine (Y) in amino-acid position 501 (N501Y) which is associated with increased binding affinity. Cluster 5 (Y453F) are variants which are believed to have been spread from minks to humans via Danish mink farms. They have moderately decreased sensitivity to neutralizing antibodies and could potentially reduce vaccine effectiveness although it is now thought that this variant is extinct following extensive mink culling and lockdown efforts. Variants of Concern include B.1.1.7 (Alpha) in the UK, B.1.351 (Beta) in South Africa, P.1 (Gamma) in Brazil and B.1.617.2 (Delta) in India.
There are a number of vaccines authorized and available for use against SARS-CoV-2 infection, including the Pfizer–BioNTech (Tozinameran – BioNTech, Pfizer, Fosun Pharma) and Moderna mRNA (mRNA-1273 – Moderna, NIAID, BARDA, CEPI) vaccines and the Oxford-AstraZeneca vaccine (AZD1222 – University of Oxford, AstraZeneca, CEPI), based on a modified chimpanzee adenovirus vector (ChAdOx1). Other vaccines available include several adenovirus-vector based vaccines (Ad5-nCoV – CanSino Biologics, Beijing Institute of Biotechnology of the Academy of Military Medical Sciences; Gam-COVID-Vac/Sputnik V – Gamaleya Research Institute of Epidemiology and Microbiology) and inactivated SARS-CoV-2 vaccines (BBIBP-CorV – Sinopharm, Beijing Institute of Biological Products, Wuhan Institute of Biological Products; BBV152 – Bharat Biotech, Indian Council of Medical Research; CoronaVac – Sinovac). Many more vaccines are in the development pipeline.
References
- Severe Acute Respiratory Syndrome Coronavirus, NCBI.
- Coronavirus. Centers for Disease Control and Prevention (CDC), 2019.
- SARS (Severe Acute Respiratory Syndrome). World Health Organization
- Anthony et al. (2017). Further Evidence for Bats as the Evolutionary Source of Middle East Respiratory Syndrome Coronavirus. Bio. 4;8(2).
- Wang et al. (2015). Evaluation of candidate vaccine approaches for MERS-CoV. Nat Commun. 28;6:7712.
- Reusken et al. (2013). Middle East respiratory syndrome coronavirus neutralising serum antibodies in dromedary camels: a comparative serological study. Lancet Infect Dis. 13(10):859-66.
- Al-Amri et al. (2017). Immunogenicity of Candidate MERS-CoV DNA Vaccines Based on the Spike Protein. Sci Rep. 23;7:44875.
- Middle East respiratory syndrome coronavirus (MERS-CoV). World Health Organization.
- Xu et al. (2019). Antibodies and vaccines against Middle East respiratory syndrome coronavirus. Emerg Microbes Infect. 8(1): 841–856.
- Novel coronavirus (2019-nCoV), World health Organisation (WHO), 2020.
- Hui et al. (2020). The continuing 2019-nCoV epidemic threat of novel coronaviruses to global health – The latest 2019 novel coronavirus outbreak in Wuhan, China. International Journal of Infectious Diseases, 91, 264–266.
- Lu R, Zhao X, Li J, et al. (2020). Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. S0140-6736(20)30251-8. doi:10.1016/S0140-6736(20)30251-8.
Human Coronavirus Antigens
We offer a range of Coronavirus antigens including native antigens and recombinant proteins for Novel Coronavirus (SARS-CoV-2, COVID-19), SARS and MERS CoV. These antigens are suitable for use in assay development, vaccine research and as antigens for the preparation of Coronavirus-specific antibodies. We also offer Horseradish peroxidase (HRP) conjugated and Biotinylated Spike proteins for assay development.
To support the investigation of SARS-CoV-2 variants, The Native Antigen Company offers a growing range of mutant Spike antigens. Expressed from our proprietary mammalian expression system, these antigens display full glycosylation and proper folding for use in the development of high-performance assays and other applications.
SARS-CoV-2 (B.1.1.529/Omicron) Stabilized Spike Glycoprotein (Trimeric), His-Strep-Tag (HEK293)
Price range: $1,048.93 through $5,385.45 excl. VAT
SARS-CoV-2 Spike Glycoproteins (S2), Sheep Fc-Tag (HEK293/CHO Cell Duo Pack)
Price range: $1,307.47 through $4,971.34 excl. VAT
SARS-CoV-2 Spike Glycoproteins (S1), Sheep Fc-Tag (HEK293/CHO Cell Duo Pack)
Price range: $1,307.47 through $4,971.34 excl. VAT
Human IgA Anti-SARS-CoV-2 Spike Antibody (A60H)
Price range: $493.99 through $1,292.77 excl. VAT
Human IgG1 Anti SARS-CoV-2 Spike (S1) Antibody (EB5)
Price range: $618.01 through $2,163.01 excl. VAT
Human IgG1 Anti SARS-CoV-2 Spike (S1) Antibody (HH10)
Price range: $618.01 through $2,163.01 excl. VAT
Human Coronavirus Antibodies
We offer Coronavirus monoclonal antibodies (including neutralizing antibodies) that are specific to SARS-CoV and SARS-CoV-2 (COVID-19) proteins, including SARS-CoV Nucleoprotein, Spike and Matrix proteins, SARS-CoV-2 Spike S2 glycoprotein and MERS-CoV Spike S1 glycoprotein.
To support the investigation of SARS-CoV-2 variants, The Native Antigen Company offers a growing range of monoclonal and polyclonal antibodies specific to Spike mutants. Our range includes antibodies that show specificity to certain Spike regions, as well as those that exhibit neutralising activity.
SARS-CoV-2 Neutralization Assay Development Kits
We are pleased to offer six different NTRL assay development kits for the identification and qualitative measurement of neutralizing antibodies for the following SARS-CoV-2 variants – Wuhan-Hu-1, Brazilian, UK, South African, Kerala and Delta.
Human ACE2 (18-615) Recombinant Protein, Sheep Fc-Tag (HEK293)
Price range: $781.96 through $2,968.09 excl. VAT
Human CD147 (BSG) Recombinant Protein, His-Tag (HEK293)
Price range: $781.96 through $2,968.09 excl. VAT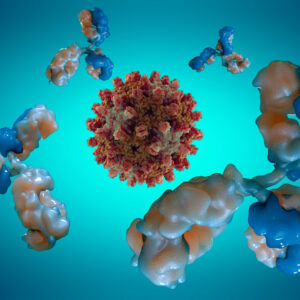
Human IgA Anti-SARS-CoV-2 Spike Antibody (A60H)
Price range: $493.99 through $1,292.77 excl. VAT
Human Coronavirus Receptors
We offer a range of human cell-surface receptors known to mediate SARS-CoV-2 host cell recognition and entry. Our recombinant proteins are produced to the highest quality, using in-house bespoke expression and purification methods.
Questions?
Check out our FAQ section for answers to the most frequently asked questions about our website and company.